how long does a heart transplant last
 How Long Do Transplanted Organs Last? - TMC News
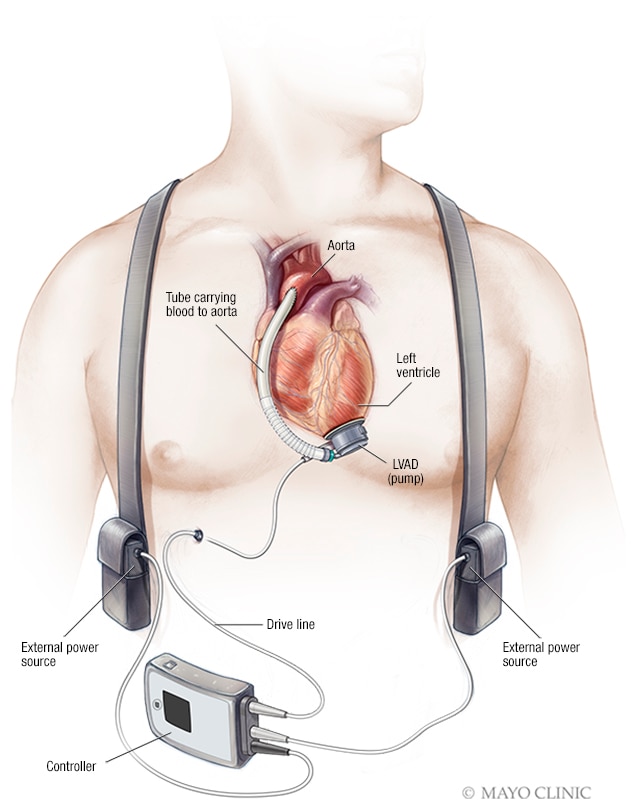
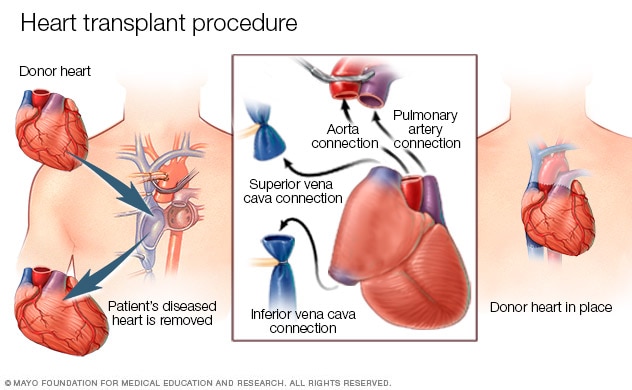
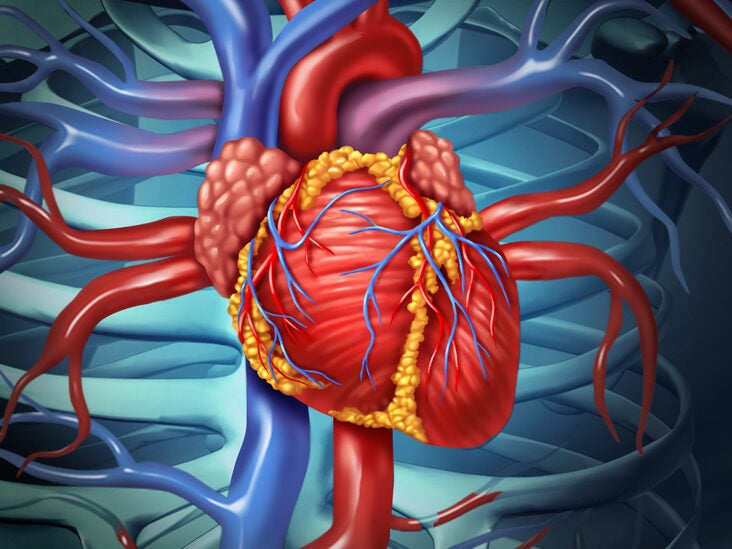
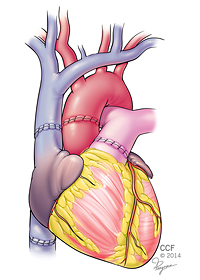
How Long Do Transplanted Organs Last? - TMC NewsDo not delay your attention in Mayo ClinicRemarked Conditions We are welcoming patients in Mayo Clinic.. Overview A heart transplant is an operation in which a sick and failed heart is replaced by a healthier donor heart. Heart transplant is a treatment that is usually reserved for people whose condition has not improved enough with medications or other surgeries. While a heart transplant is an important operation, its probability of survival is good with proper follow-up care. Products " Services " Why is it doneHeart transplants are performed when other treatments for heart problems have not worked, leading to heart failure. In adults, heart failure can be caused by:In children, heart failure is most often caused by a congenital heart defect or cardiomyopathy. Another organ transplant can be done at the same time as a heart transplant (multiorgan transplant) in people with certain conditions in select medical centers. Multiorganic transplants include: However, a heart transplant is not suitable for everyone. You may not be a good candidate for a heart transplant if you: Left ventricular assistance device (LVAD) Left ventricular assistance device (LVAD)A left ventricular assistance device (LVAD) is implanted in the chest. Helps pump blood from the left ventricle of your heart and the rest of your body. A control unit and battery pack are used outside your body and are connected to the LVAD through a port on your skin. For some people who cannot have a heart transplant, another option may be a ventricular assistance device (VAD). A ventricular assist device is a mechanical pump implanted in the chest that helps pump blood from the lower chambers of the heart (ventricles) to the rest of the body. VADs are commonly used as temporary treatments for people who expect heart transplants. These devices are increasingly used as long-term treatments for people who have heart failure but are not eligible for heart transplants. If a VAD does not help your heart, doctors may sometimes consider a total artificial heart — a device that replaces your heart's ventricles — as a short-term alternative treatment while waiting for a heart transplant. Risks In addition to the risks of open heart surgery, including bleeding, infection, and blood clots, the risks of a heart transplant include: I reject the donor heart. One of the most important risks after a heart transplant is your body rejecting the donor heart. Your immune system can see your donor heart as a foreign object and try to reject it, which can damage your heart. Each heart transplant receives medication to prevent rejection (immunosuppressive), and as a result, the rejection rate continues to decline. Sometimes a change in medications will stop the rejection if it happens. To help prevent rejection, it is critical that you always take your medications as prescribed and keep all your appointments with your doctor. Rejection often occurs without symptoms. To determine if your body is rejecting the new heart, you will have frequent heart biopsies during the first year after your transplant. After that, you don't need biopsies so often. During the biopsy, a tube is inserted into a vein in the neck or groin and is directed to your heart. A biopsy device is run through the tube to take a small sample of heart tissue, which is examined in a laboratory. How to PreparePreparations for a heart transplant often begin weeks or months before receiving a donor heart. Taking the first steps If your doctor recommends a heart transplant, you are likely to be referred to a heart transplant center for evaluation. Or you can select a transplant center on your own. Check your health insurance to see which transplant centers are covered in your plan. When evaluating a heart transplant center, consider the number of heart transplants that a center performs every year and survival rates. You can compare transplant center statistics using a database maintained by the . You should also check if a transplant center offers other services you may need. These include coordinating support groups, helping with travel arrangements, helping you find local homes for your recovery period or directing you to organizations that can help with these concerns. Once you decide in a center, you will have to have an evaluation to see if it is eligible for a transplant. The evaluation will check if: Expecting a donor organ If the medical team at the transplant center determines that you are a good candidate for a heart transplant, the center will put you on a waiting list. Waiting can be long as there are more people who need hearts than donors. Finding a donor depends on its size, its type of blood and its disease. While you are on the waiting list, your medical team will monitor your heart and other organs and adjust your treatment as needed. The team will help you learn to care for your heart by eating well and being active. If medical therapy does not support your vital organs while waiting for a donor heart, your doctors may recommend that you have an implanted device to support your heart while waiting for a donor organ. These devices are known as ventricular assist devices (VAD). Devices are also called transplant bridges because they earn time to wait until a donor heart is available. Immediately before transplant surgery A heart transplant usually needs to occur within four hours of organ removal so that the donor organ remains usable. As a result, hearts are first offered to a transplant center near and then to centers within certain distances of the donor hospital. The transplant center will provide you with a poster or cell phone to notify you when a potential heart is available. You should keep your cell phone or laptop loaded and on at all times. Once you are notified, you and your transplant team have limited time to accept donation. You'll have to go to the transplant hospital immediately after being notified. As much as possible, make travel plans before time. Some heart transplant centers provide private air transportation or other travel arrangements. Have a suitcase full of everything you will need for your stay in the hospital, as well as an extra supply of your medications 24 hours a day. Once you arrive at the hospital, your doctors and your transplant team will perform a final evaluation to determine if the donor heart is suitable for you and if you are ready for surgery. If your doctors and your transplant team decide that the donor heart or surgery is not appropriate for you, you may not have the transplant. Mayo doctors and staff can receive donor organs from other places and transport them to prepare for the transplant. What You Can Expect During the Procedure Mayo Clinic's heart surgeons work with a team to perform heart transplant surgery. Heart transplant surgery is an open heart procedure that lasts several hours. If you have had previous heart surgery, surgery is more complicated and it will take longer. You will receive a medicine that will make you sleep (general anesthesia) before the procedure. Your surgeons will connect you to a heart lung bypass machine to keep your blood rich in oxygen flowing through your body. Your surgeon will make an incision in your chest. Your surgeon will separate your bone from your chest and open your rib cage so you can operate in your heart. Your surgeon then removes the sick heart and takes the donor heart instead. Next, attach the main blood vessels to the donor heart. The new heart often begins to beat when the flow of blood is restored. Sometimes an electrical discharge is needed so that the donor's heart is beat properly. You will be given medication to help with pain control after surgery. You will also have a fan to help you breathe and tubes in your chest to drain fluids from around your lungs and heart. After surgery, you will also receive fluids and medicines through intravenous tubes (IV). After the procedure Initially you will stay in the intensive care unit (IU) for a few days, then you will move to a regular hospital room. He's probably staying in the hospital for a week or two. The time spent at ICU and hospital varies from person to person. After leaving the hospital, your transplant team will monitor you at your outpatient transplant center. Due to the frequency and intensity of monitoring, many people remain close to the transplant center during the first three months. Afterwards, follow-up visits are less frequent, and it is easier to travel back and forth. You will also be watched for any signs or symptoms of rejection, such as shortness of breath, fever, fatigue, not urinating as much or weight gain. It is important that your transplant team know if you notice any signs or symptoms of rejection or infection. To determine if your body is rejecting the new heart, you will have frequent heart biopsies in the first months after heart transplant, when rejection is more likely to occur. The frequency of the necessary biopsies decreases over time. During a heart biopsy, a doctor inserts a tube into a vein in the neck or groin and directs it to your heart. The doctor administers a biopsy device through the tube to extract a small sample of heart tissue, which is examined in a laboratory. You'll have to make several long-term adjustments after you had your heart transplant. These include:Taking immunosuppressants. These medicines decrease the activity of your immune system to prevent you from attacking your donated heart. You'll take some of these medications for the rest of your life. Because immunosuppressants make your body more vulnerable to infection, your doctor may also prescribe antibacterial, antiviral and antifungal medications. Some medicines may get worse — or increase the risk of developing — conditions such as high blood pressure, high cholesterol, cancer, or diabetes. Over time, as the risk of rejection decreases, doses and the number of anti-rejection drugs can be reduced. Drug management, therapies and a permanent care plan. After a heart transplant, taking all your medications while your doctor instructs and following a permanent care plan is vital. Your doctor may give you instructions on your lifestyle, such as using sunscreen, not using tobacco products, exercising, eating a healthy diet, and taking care to reduce your risk of infection. Follow all instructions from your doctor, consult your doctor regularly for follow-up appointments, and tell your doctor if you have signs or symptoms of complications. It's a good idea to set up a daily routine to take your medications so you don't forget. Keep a list of all your medications with you at all times in case you need emergency medical care, and tell all your doctors what you take every time a new medication is prescribed. Heart Transplant Procedure Heart Transplantation Procedure In a heart transplant procedure, a surgeon removes the heart from the disease and takes the donor heart instead. Next, attach the main blood vessels to the donor heart. Most people receiving a heart transplant enjoy good quality of life. Depending on your condition, you can resume many of your daily life activities, such as going back to work, taking part in hobbies and sports and exercising. Discuss with your doctor what activities are appropriate for you. Some women who have had heart transplants may become pregnant. However, talk to your doctor if you are considering having children after your transplant. You may need medication settings before you become pregnant, as some medicines may cause complications in your pregnancy. Survival rates after heart transplant vary according to several factors. Survival rates continue to improve despite an increase in older and higher risk heart transplant receptors. Worldwide, the global survival rate is more than 85% after a year and about 69% after five years for adults. What if your new heart fails? Heart transplants are not successful for everyone. Your new heart may fail for several reasons. Your doctor may recommend adjusting your medications or, in more extreme cases, having another heart transplant. If the additional treatment options are limited, you may choose to stop the treatment. Discussions with your heart transplant team, doctor and family should address your expectations and preferences for treatment, emergency care and end-of-life care. Clinical trials testing and procedures to help prevent, detect, treat or manage conditions. Copying and Support It is normal to feel anxious or overwhelmed by waiting for a transplant or being afraid of rejection, back to work or other problems after a transplant. Finding support from friends and family can help you cope during this stressful time. Diet and Nutrition After your heart transplant, you may need to adjust your diet to keep your heart healthy and working well. Maintaining a healthy weight through diet and exercise can help avoid complications such as high blood pressure, heart disease, and diabetes. A nutrition specialist (dietitian) can discuss your nutrition and diet needs and answer any questions you have after your transplant. Your dietitian will provide you with several healthy food options and ideas to use in your food plan. Your dietitian's recommendations may include: Exercise After your heart transplant, your doctor and your treatment team may recommend that you exercise and perform a regular part of your life to further improve your overall physical and mental health. Exercise can regularly help you control your blood pressure, reduce stress, maintain a healthy weight, strengthen your bones and increase your physical function. Your treatment team will create an exercise program designed to meet your individual needs and goals. You will participate to improve your strength, strength and energy. Heart rehabilitation incorporates education and exercise to help you improve your health and recover after your heart transplant. Your exercise program may include warmup exercises such as stretching or slow walk. Your treatment team may suggest physical activities such as walking, cycling and force training as part of your exercise program. Specialists on the treatment team will probably recommend you to cool after exercising, maybe walking slowly. Discuss with your treatment team what activities may be appropriate for you. Take a break from exercising if you feel tired. If you feel symptoms such as shortness of breath, nausea, irregular heart rate or dizziness, stop exercising. If your symptoms do not go away, contact your doctor immediately. Related news of Mayo ClinicProducts & Services Mayo Clinic in Rochester, Minn., has been recognized as one of the best hospitals of Cardiology and Heart Surgery in the nation by 2020-2021 by the U.S. World News Report. Heart transplant Advert Mayo Clinic does not support companies or products. Advertising revenues support our non-profit mission. Mayo Clinic Market Take a look at these best-sellers and special offers in Mayo Clinic books and newsletters. Any use of this site constitutes your agreement with the following Terms and Conditions and the Privacy Policy. A single copy of these materials can be reprinted for non-commercial personal use only. "Mayo", "Mayo Clinic", "MayoClinic.org", "Mayo Clinic Healthy Living", and the Mayo Clinic triple shield logo are trademarks of the Mayo Foundation for Medical Education and Research. This site complies with the information:
Dick Cheney Surgery: 7 Essential Facts about Heart Transplants

How Long Do Transplanted Organs Last? - TMC News

Matching Donors and Recipients | Organ Donor

40 years of heart transplant - timeline | BHF
Heart transplant - Mayo Clinic

How long can a heart survive after being removed from a donor's body? | Heart Transplant - Sharecare

10 Things Your Doctor Won't Tell You About Transplants | Everyday Health
The Crucial Hours of a Heart Transplant | The Well by Northwell

He had 2 heart transplants. At 43, as a new dad, he needed a third
Not waiting around to die: Considering my prognosis after a heart transplant - The DO

Living for Years Without a Heart Is Now Possible
Heart transplant - Mayo Clinic
Two hearts are better than one for toddler who undergoes historic operation

Baby Lincoln was in 'his last days,' then a new heart arrived | The Seattle Times
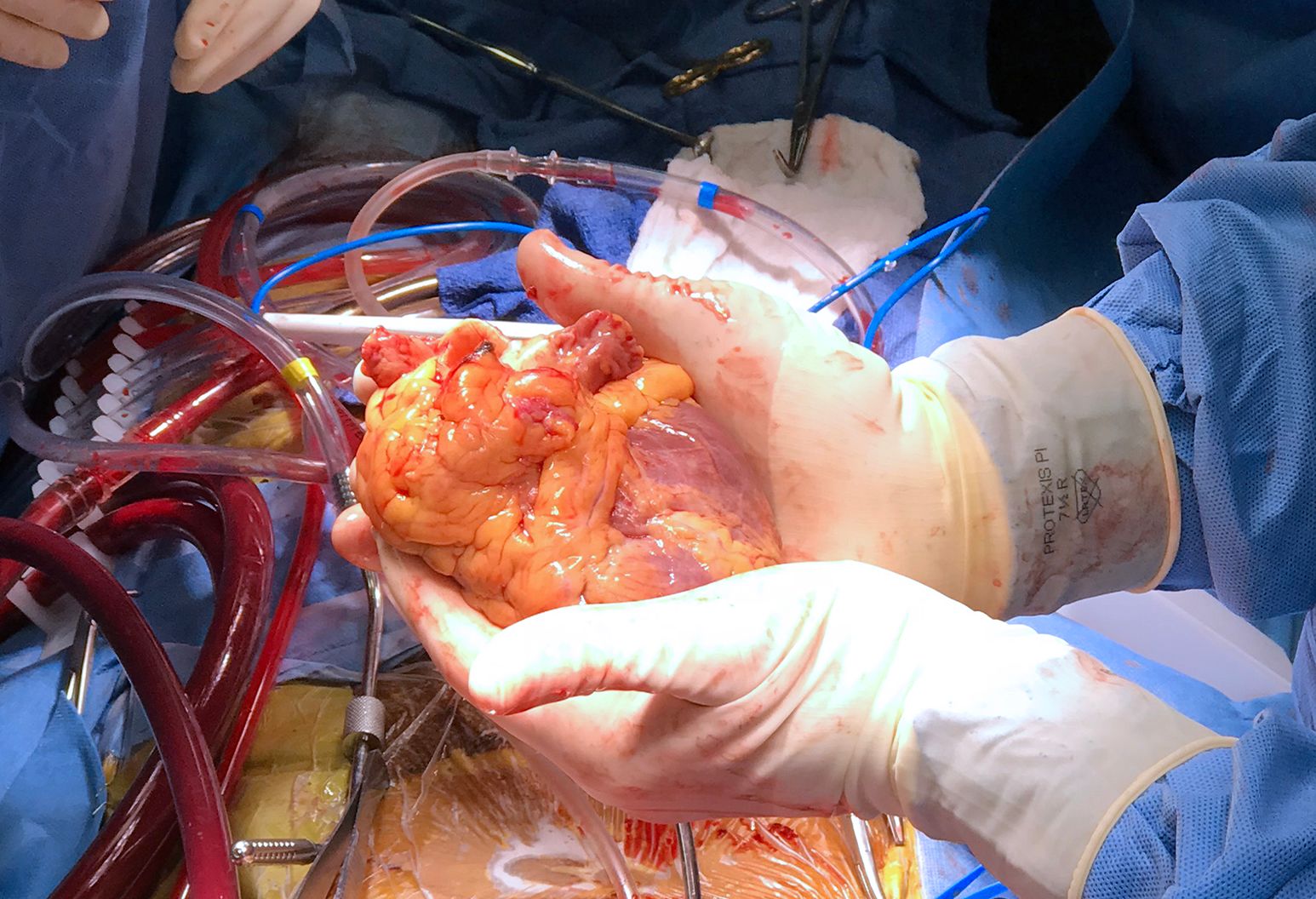
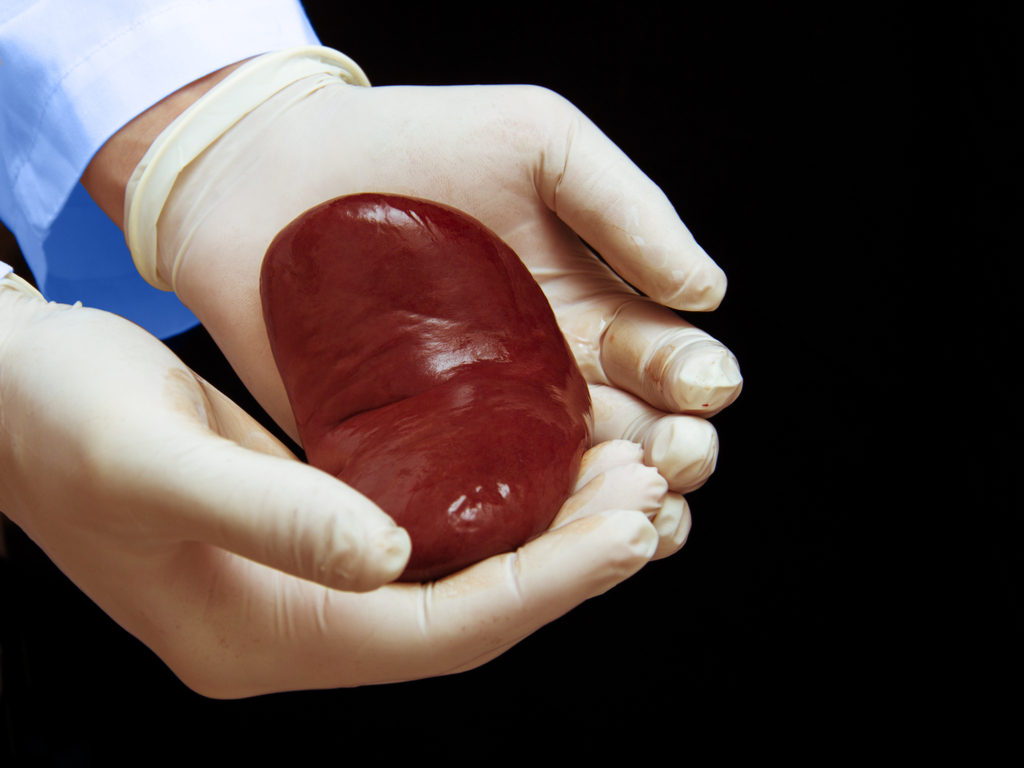
Picture of my friend holding his old heart. He had a heart transplant last August. He passed away a few days ago. : pics

Characteristics of Patients With Survival Longer Than 20 Years Following Heart Transplantation | Revista Española de Cardiología (English Edition)
Liver transplant survival rate: Statistics and recovery
Heart Transplant Surgery: Procedure, Costs, Life Expectancy, and More

The First Artificial Heart, 30 Years Later | University of Utah Health
How long does a heart transplant surgery take?
Heart Transplant

Heart Transplant Surgery: Procedure, Costs, Life Expectancy, and More

Heart transplantation - Wikipedia

About That Heart Device Your Doctor Recommends: Are You Sure You Understand The Risks? | CommonHealth

Everything you need to know about organ transplants
How Long Can Organs Stay Outside the Body Before Being Transplanted? | Live Science
Heart Transplant | Johns Hopkins Medicine

How Long Do Transplanted Organs Last? - TMC News

Lung transplantation - Wikipedia
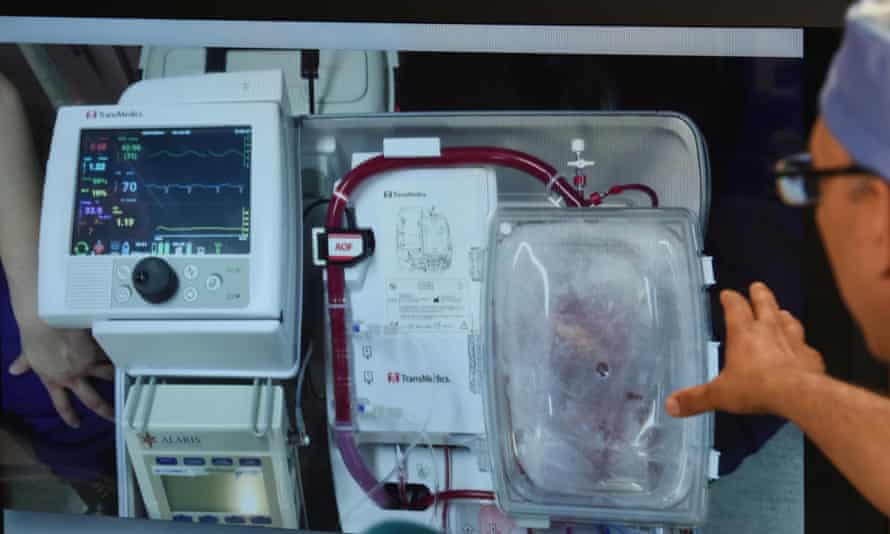
Success for first non-beating heart transplant in Europe | Science | The Guardian

How long do transplanted organs last? | Ohio State Medical Center

Living for Years Without a Heart Is Now Possible
No Cash, No Heart. Transplant Centers Require Proof Of Payment. | Kaiser Health News

Student has heart transplant after her tiredness became deadly | Daily Mail Online
Getting a new heart and a new lease of life - SingHealth
How long does it typically take for an organ to travel from donor to reciever? - Quora

Why Your Odds of Getting a Heart Transplant Are So Low | Time
A terrible crime, a patient waiting for a transplant: The tragic, redemptive journey of one heart - The Washington Post

How Long Does Heart Bypass Surgery Last? • MyHeart
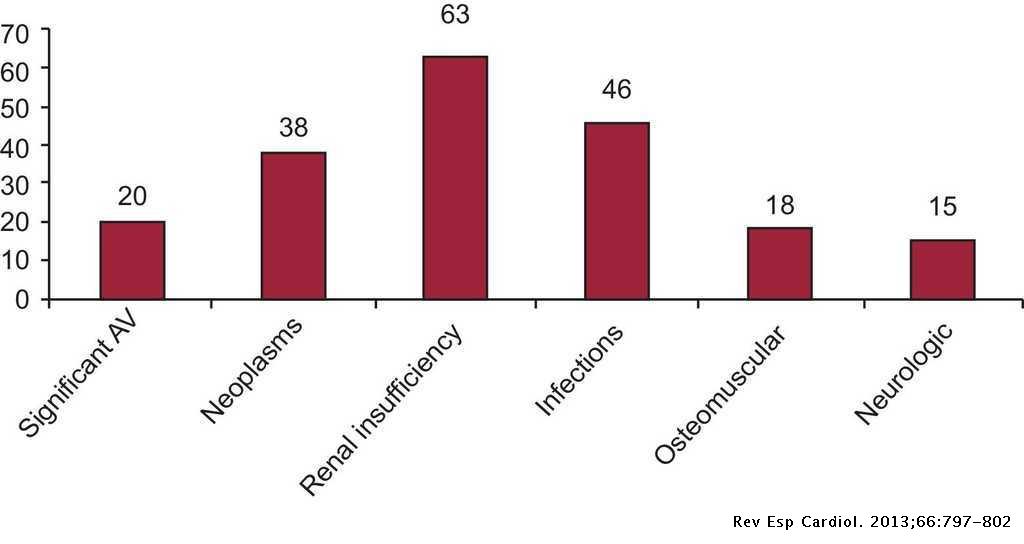
Characteristics of Patients With Survival Longer Than 20 Years Following Heart Transplantation | Revista Española de Cardiología (English Edition)
Posting Komentar untuk "how long does a heart transplant last"